Program Project Grant (P01): Translational Studies in FLASH Particle Radiotherapy
NIH Grant # P01-CA257904-01
Contact Principal Investigator:
- Costas Koumenis, PhD, University of Pennsylvania
Co- Principal Investigator:
- Alex Lin, MD, University of Pennsylvania
Project Overview:
Radiation therapy (RT) is used in the curative setting for many cancers including sarcomas and lung and pancreatic cancer. Despite significant improvements over the past few decades, there is still much room for improvement as patients still develop RT-induced injuries or second malignant neoplasms. FLASH radiotherapy, which delivers a large dose of radiation at an ultra-high dose rate could potentially reduce toxicity. Our overall hypothesis is that Proton/Carbon Particle FLASH RT is superior to Standard Particle RT in protecting normal tissues while the two modalities will be equipotent in controlling malignant growth. Project 1, which focuses on pancreatic cancer, will define the dosimetric and biophysical parameters that will maximally spare normal intestine tissues using FLASH proton therapy (F-PRT) without compromising antitumor effects. It will delineate mechanistic aspects of differential response of normal intestinal tissues, by focusing on the relative sparing of the stem/progenitor cell population. Project 1 will also employ p53+/- transgenic mouse models to dissect the genetic determinants of differential GI toxicity of Standard proton therapy (S-PRT) vs F-PRT. Project 2 will explore the ability of F-PRT to ameliorate adverse events (inflammation, fibrosis, lymphedema, changes to bone structure, radiation-induced cancers) that pose barriers to the treatment of sarcomas with RT. We will also carry out a phase 1/2 trial that will treat canine patients with osteosarcomas definitively with F-PRT. Project 3 will compare the efficacy of FLASH-RT given with carbon ion radiotherapy (CRT) vs. standard dose rate and compare it to electron F-RT. Studies will focus on the mitigation of normal tissue injury in NSCLC with an emphasis on the impact of normal tissue and intratumoral hypoxia to response following C-RT. Lastly, Project 4 will develop and validate the use of pencil beam scanning (PBS) technology for particle F-RT. It will analyze spatiotemporal variations and SOBP (spread out Bragg peak) vs. shoot through PBS and develop dose delivery algorithms for modeling biological effects for PBS-based FLASH proton therapy. These tools will be incorporated in the experimental plans of project 1-3. These Projects are supported by 4 Cores including an Administrative Core (Core A), Physics-Dosimetry Core (Core B), which will offer infrastructure services to harmonize dosimetry between various sites and a Comparative Pathology core (Core C) for tissue preparation for histopathological evaluation. Statistical services will be provided by Core D. Collectively, this highly integrated effort led by recognized leaders in Radiation and Tumor Biology, aims to define the biological, dosimetric and biophysical parameters and molecular mechanisms under which FLASH RT is most effective in tumors and tissues we deem the most likely to be first tested in clinical trials. It is our belief that only by acquiring this knowledge will this exciting and novel modality be ushered into the clinic in a safe and effective manner to improve therapeutic outcome and quality of life of cancer patients
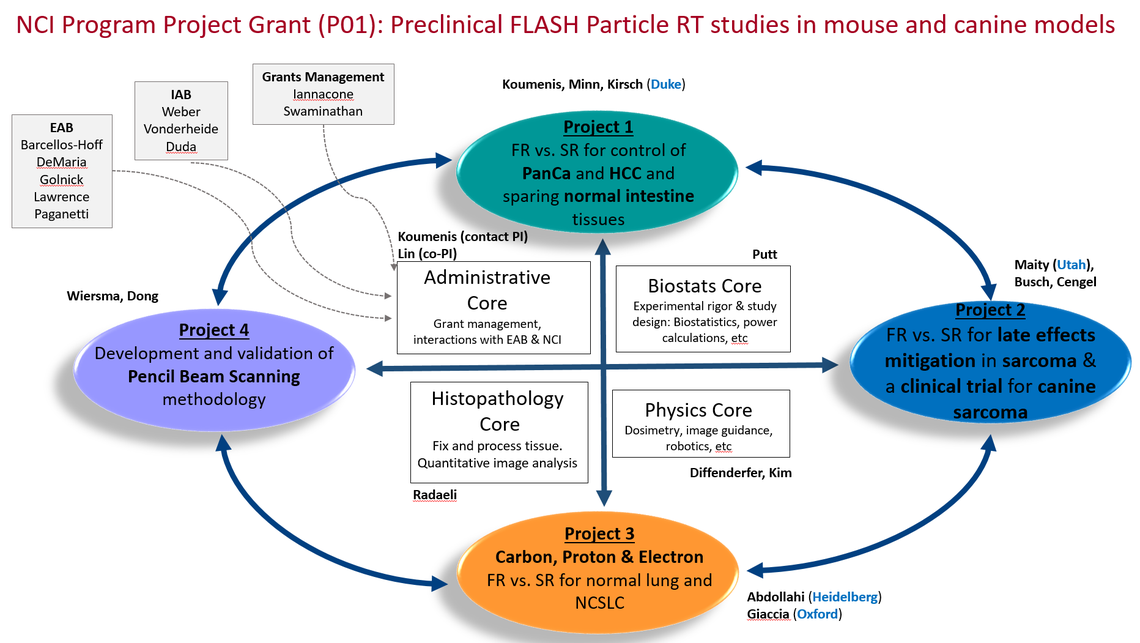
Project 1: FLASH vs. Standard radiotherapy for treatment of PDAC and sparing normal intestine tissues
Project 1 will define the dosimetric and biophysical parameters that maximize normal tissue sparing and antitumor effects of F-PRT, by performing dose-escalation studies in syngeneic models; it will investigate mechanisms of differential response of normal intestinal tissues to standard proton radiotherapy (S-PRT) vs FLASH proton radiotherapy (F-PRT) using single-cell transcriptomics and genetic mouse models
Project 2: Mitigation of radiation toxicity in treatment of sarcoma with FLASH vs. Standard dose rates
Project 2 will use murine models to: (i) understand when and how F-PRT can lead to reduced inflammation, lymphedema, fibrosis, and vascular effects and (ii) define the clinical uses of F-PRT to avoid second malignancies that can be associated with S-PRT and exploit its positive impact on therapeutic window when employed in combination with surgery. Finally, Project 2 will conduct a phase 1-2 trial using FLASH radiation in the definitive setting (no surgery) for osteosarcomas in dogs.
Project 3: Carbon vs. Electron FLASH radiotherapy for mitigation of normal lung injury in treatment of NSCLC
Project 3 will compare FLASH dose-rate RT generated with electrons (Oxford) and carbon (Heidelberg) and compare to protons (UPenn) to provide evidence for equipotency of FLASH vs. standard RT to tumor growth control, while sparing normal tissues (lung, vascular, heart and esophagus) in preclinical models of thoracic irradiation. Interaction with online O2 monitoring (Oxford) combined with the ability to modulate LET with carbon ions (Heidelberg) will provide a unique ability to dissect the impact of oxygen on FLASHeffects.
Project 4 : Development and validation of Pencil Beam Scanning methodology for proton FLASH radiotherapy
Project 4 will (i) establish a beam-control system for the research beamline to create a variable dose rate delivery to simulate the spatiotemporal nature of pencil beam scanning (PBS), (ii) compare FLASH effects at the high LET Spread-Out-Bragg Peak (SOBP) with those at the entrance region, (iii) develop a dose model to investigate the potential biological effects related to the high instantaneous dose rate and dynamic beam delivery scheme in PBS, (iv) develop real-time dose rate monitoring system and high-speed dose recording to ensure accurate F-PRT dose delivery and (v) develop FLASH-specific quality assurance procedures.
Core A: Administrative: coordinates administrative and financial aspects of the collaboration, oversee day-to-day operations globally (Oxford, Heidelberg), and the US (UPenn and Duke) and organize EAB meetings, symposia, and annual reporting to the NCI.
Core B: Physics-Dosimetry will offer infrastructure services to (i) perform the RT studies at Penn, (ii) ensure physical dose between proton/carbon/electron and FLASH/standard and (iii) develop animal-specific treatment planning for mice and dogs. Critically, it will also develop and implement approaches for harmonization of dosimetry between the various sites.
Core C: Comparative Pathology located at UPenn Vet School, will provide services including tissue preparation for histopathological evaluation, optimized immunofluorescence and IHC staining of immune infiltrates, histochemical stains (e.g. trichrome), and quantitative image analysis.
Core D: Biostatistics will help develop rigorous study designs and analytic plans appropriate for the research goals of each project. It will also provide resources need to assess sample size and statistical power, with particular attention to the dog study in Project 2
External Advisory Board:
Internal Advisory Board:
Calendar of Events:
FLASH P01 Monthly Meeting: the first Friday of every month at 9:00AM
Publications:
|
|
Karle C, Liew H, Tessonnier T, Mein S, Petersson K, Schömers C, Scheloske S, Brons S, Cee R, Major G, Haberer T, Abdollahi A, Debus J, Dokic I, Mairani A. Oxygen consumption measurements at ultra-high dose rate over a wide LET range. Med Phys. 2025 Feb;52(2):1323-1334. doi: 10.1002/mp.17496. Epub 2024 Nov 6. PubMed PMID: 39504410; PubMed Central PMCID: PMC11788059.
Lim TL, Morral C, Verginadis II, Kim K, Luo L, Foley CJ, Kim MM, Li N, Yoshor B, Njah K, Putt M, Oliaei Motlagh SA, Velalopoulou A, Chowdhury P, Bicher S, Goia D, Lengner CJ, Wrana JL, Koumenis C, Minn AJ. Early Inflammation and Interferon Signaling Direct Enhanced Intestinal Crypt Regeneration after Proton FLASH Radiotherapy. bioRxiv. 2024 Aug 19;. doi: 10.1101/2024.08.16.608284. PubMed PMID: 39229237; PubMed Central PMCID: PMC11370362.
Kim K, Kim MM, Skoufos G, Diffenderfer ES, Motlagh SAO, Kokkorakis M, Koliaki I, Morcos G, Shoniyozov K, Griffin J, Hatzigeorgiou AG, Metz JM, Lin A, Feigenberg SJ, Cengel KA, Ky B, Koumenis C, Verginadis II. FLASH Proton Radiation Therapy Mitigates Inflammatory and Fibrotic Pathways and Preserves Cardiac Function in a Preclinical Mouse Model of Radiation-Induced Heart Disease. Int J Radiat Oncol Biol Phys. 2024 Jul 15;119(4):1234-1247. doi: 10.1016/j.ijrobp.2024.01.224. Epub 2024 Feb 15. PubMed PMID: 38364948; PubMed Central PMCID: PMC11209795.
Verginadis II, Velalopoulou A, Kim MM, Kim K, Paraskevaidis I, Bell B, Oliaei Motlagh SA, Karaj A, Banerjee E, Finesso G, Assenmacher CA, Radaelli E, Lu J, Lin Y, Putt ME, Diffenderfer ES, Guha C, Qin L, Metz JM, Maity A, Cengel KA, Koumenis C, Busch TM. FLASH proton reirradiation, with or without hypofractionation, mitigates chronic toxicity in the normal murine intestine, skin, and bone. bioRxiv. 2024 Jul 11;. doi: 10.1101/2024.07.08.602528. PubMed PMID: 39026805; PubMed Central PMCID: PMC11257476.
Chowdhury P, Velalopoulou A, Verginadis II, Morcos G, Loo PE, Kim MM, Motlagh SAO, Shoniyozov K, Diffenderfer ES, Ocampo EA, Putt M, Assenmacher CA, Radaelli E, Lu J, Qin L, Liu H, Leli NM, Girdhani S, Denef N, Vander Stappen F, Cengel KA, Busch TM, Metz JM, Dong L, Lin A, Koumenis C. Proton FLASH Radiotherapy Ameliorates Radiation-induced Salivary Gland Dysfunction and Oral Mucositis and Increases Survival in a Mouse Model of Head and Neck Cancer. Mol Cancer Ther. 2024 Jun 4;23(6):877-889. doi: 10.1158/1535-7163.MCT-23-0663. PubMed PMID: 38593239; PubMed Central PMCID: PMC11148539.
Morral C, Ayyaz A, Kuo HC, Fink M, Verginadis II, Daniel AR, Burner DN, Driver LM, Satow S, Hasapis S, Ghinnagow R, Luo L, Ma Y, Attardi LD, Koumenis C, Minn AJ, Wrana JL, Lee CL, Kirsch DG. p53 promotes revival stem cells in the regenerating intestine after severe radiation injury. Nat Commun. 2024 Apr 8;15(1):3018. doi: 10.1038/s41467-024-47124-8. PubMed PMID: 38589357; PubMed Central PMCID: PMC11001929.
Rank L, Dogan O, Kopp B, Mein S, Verona-Rinati G, Kranzer R, Marinelli M, Mairani A, Tessonnier T. Development and benchmarking of a dose rate engine for raster-scanned FLASH helium ions. Med Phys. 2024 Mar;51(3):2251-2262. doi: 10.1002/mp.16793. Epub 2023 Oct 17. PubMed PMID: 37847027; PubMed Central PMCID: PMC10939952.
El Khatib M, Motlagh AO, Beyer JN, Troxler T, Allu SR, Sun Q, Burslem GM, Vinogradov SA. Direct Measurements of FLASH-Induced Changes in Intracellular Oxygenation. Int J Radiat Oncol Biol Phys. 2024 Mar 1;118(3):781-789. doi: 10.1016/j.ijrobp.2023.09.019. Epub 2023 Sep 18. PubMed PMID: 37729972; PubMed Central PMCID: PMC11474819.
Tessonnier T, Verona-Rinati G, Rank L, Kranzer R, Mairani A, Marinelli M. Diamond detectors for dose and instantaneous dose-rate measurements for ultra-high dose-rate scanned helium ion beams. Med Phys. 2024 Feb;51(2):1450-1459. doi: 10.1002/mp.16757. Epub 2023 Sep 24. PubMed PMID: 37742343; PubMed Central PMCID: PMC10922163.
Koch CJ, Kim MM, Wiersma RD. Radiation-Chemical Oxygen Depletion Depends on Chemical Environment and Dose Rate: Implications for the FLASH Effect. Int J Radiat Oncol Biol Phys. 2023 Sep 1;117(1):214-222. doi: 10.1016/j.ijrobp.2023.04.001. Epub 2023 Apr 13. PubMed PMID: 37059234; PubMed Central PMCID: PMC11044555. select Zou W, Zhang R, Schüler E, Taylor PA, Mascia AE, Diffenderfer ES, Zhao T, Ayan AS, Sharma M, Yu SJ, Lu W, Bosch WR, Tsien C, Surucu M, Pollard-Larkin JM, Schuemann J, Moros EG, Bazalova-Carter M, Gladstone DJ, Li H, Simone CB 2nd, Petersson K, Kry SF, Maity A, Loo BW Jr, Dong L, Maxim PG, Xiao Y, Buchsbaum JC. Framework for Quality Assurance of Ultrahigh Dose Rate Clinical Trials Investigating FLASH Effects and Current Technology Gaps. Int J Radiat Oncol Biol Phys. 2023 Aug 1;116(5):1202-1217. doi: 10.1016/j.ijrobp.2023.04.018. Epub 2023 Apr 28. Review. PubMed PMID: 37121362; PubMed Central PMCID: PMC10526970.
Tan HS, Teo KBK, Dong L, Friberg A, Koumenis C, Diffenderfer E, Zou JW. Modeling ultra-high dose rate electron and proton FLASH effect with the physicochemical approach. Phys Med Biol. 2023 Jul 10;68(14). doi: 10.1088/1361-6560/ace14d. PubMed PMID: 37352867; PubMed Central PMCID: PMC10472835.
Kim MM, Zou W. Ultra-high dose rate FLASH radiation therapy for cancer. Med Phys. 2023 Jun;50 Suppl 1(Suppl 1):58-61. doi: 10.1002/mp.16271. Epub 2023 Feb 21. Review. PubMed PMID: 36758965; PubMed Central PMCID: PMC11056953.
Cooper CR, Jones DJL, Jones GDD, Petersson K. Comet Assay Profiling of FLASH-Induced Damage: Mechanistic Insights into the Effects of FLASH Irradiation. Int J Mol Sci. 2023 Apr 13;24(8). doi: 10.3390/ijms24087195. PubMed PMID: 37108360; PubMed Central PMCID: PMC10138874.
Liew H, Mein S, Tessonnier T, Abdollahi A, Debus J, Dokic I, Mairani A. Do We Preserve Tumor Control Probability (TCP) in FLASH Radiotherapy? A Model-Based Analysis. Int J Mol Sci. 2023 Mar 7;24(6). doi: 10.3390/ijms24065118. PubMed PMID: 36982185; PubMed Central PMCID: PMC10049554.
Zou W, Kim H, Diffenderfer ES, Carlson DJ, Koch CJ, Xiao Y, Teo BK, Kim MM, Metz JM, Fan Y, Maity A, Koumenis C, Busch TM, Wiersma R, Cengel KA, Dong L. A phenomenological model of proton FLASH oxygen depletion effects depending on tissue vasculature and oxygen supply. Front Oncol. 2022;12:1004121. doi: 10.3389/fonc.2022.1004121. eCollection 2022. PubMed PMID: 36518319; PubMed Central PMCID: PMC9742361.
Maity A, Koumenis C. Shining a FLASHlight on Ultrahigh Dose-Rate Radiation and Possible Late Toxicity. Clin Cancer Res. 2022 Sep 1;28(17):3636-3638. doi: 10.1158/1078-0432.CCR-22-1255. PubMed PMID: 35736814; PubMed Central PMCID: PMC9444945.
Van Slyke AL, El Khatib M, Velalopoulou A, Diffenderfer E, Shoniyozov K, Kim MM, Karagounis IV, Busch TM, Vinogradov SA, Koch CJ, Wiersma RD. Oxygen Monitoring in Model Solutions and In Vivo in Mice During Proton Irradiation at Conventional and FLASH Dose Rates. Radiat Res. 2022 Aug 1;198(2):181-189. doi: 10.1667/RADE-21-00232.1. PubMed PMID: 35640166; PubMed Central PMCID: PMC10176203.
Dokic I, Meister S, Bojcevski J, Tessonnier T, Walsh D, Knoll M, Mein S, Tang Z, Vogelbacher L, Rittmueller C, Moustafa M, Krunic D, Brons S, Haberer T, Debus J, Mairani A, Abdollahi A. Neuroprotective Effects of Ultra-High Dose Rate FLASH Bragg Peak Proton Irradiation. Int J Radiat Oncol Biol Phys. 2022 Jul 1;113(3):614-623. doi: 10.1016/j.ijrobp.2022.02.020. Epub 2022 Feb 20. PubMed PMID: 35196536; PubMed Central PMCID: PMC11034835.
Niklas M, Schlegel J, Liew H, Zimmermann F, Rein K, Walsh DWM, Dzyubachyk O, Holland-Letz T, Rahmanian S, Greilich S, Runz A, Jäkel O, Debus J, Abdollahi A. Biosensor for deconvolution of individual cell fate in response to ion beam irradiation. Cell Rep Methods. 2022 Feb 28;2(2):100169. doi: 10.1016/j.crmeth.2022.100169. eCollection 2022 Feb 28. PubMed PMID: 35474967; PubMed Central PMCID: PMC9017136. |
|
|

